Estimated reading time: 4 minutes
Varicose veins is a common condition that affects millions of people worldwide and can sometimes indicate more serious health issues. Knowing when to worry about varicose veins is crucial for maintaining vascular health and preventing any future complications.
In this blog, we’ll explore the signs and symptoms that may need extra attention.

Private varicose veins treatment at a glance
- Procedure time: procedure dependent
- Hospital stay: day-case or overnight
- Anaesthetic type: local or general
- Price: £395 – £4,499 (surgery dependent)
- Payment options: self-pay, finance, or insured
What are varicose veins and why do they occur?
Varicose veins are enlarged, swollen, and twisted veins that usually appear blue or dark purple. They can occur in any vein that is close to the skin’s surface, but are most commonly found in the legs and feet. Varicose veins develop when the valves in the veins weaken or become damaged, causing blood to pool and the veins to bulge.
Risk factors
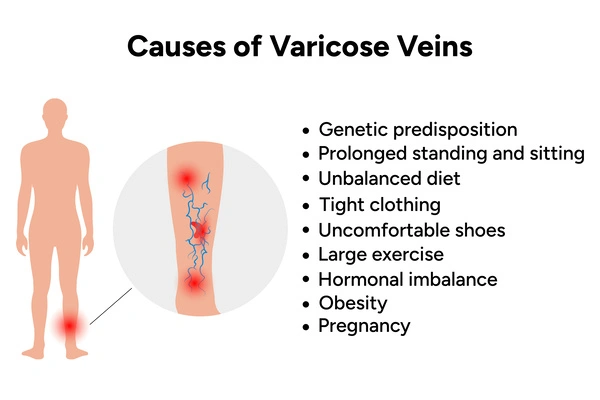
Several risk factors increase the likelihood of developing varicose veins. These include:
- Family history: If one or both parents have varicose veins, they are more likely to develop in their children
- Age: The risk of developing them increases as you get older, as the veins lose elasticity and the valves weaken over time
- Gender: Women are more likely to develop varicose veins than men
- Pregnancy: Pregnancy increases the risk of varicose veins due to the pressure exerted by the growing uterus. Hormonal changes also affect vein health and can lead to the development of varicose veins
- Obesity: Excess weight puts added pressure on the veins in your legs. This makes it harder to carry blood upward toward the heart
- Prolonged standing or sitting: Jobs or activities that involve long periods of standing or sitting can increase the risk of varicose veins. When you remain in one position for extended periods, blood pools in the veins, putting strain on the vessel walls and valves
- Previous history of blood clots: People who have had blood clots in the past may be at a higher risk of developing varicose veins. Blood clots can damage the veins and valves, leading to vein dysfunction
- Other medical conditions: Certain medical conditions (such as chronic venous insufficiency, deep vein thrombosis, or vascular malformations) can increase the risk of varicose veins.
Are all varicose veins dangerous?
No, not necessarily. Many people experience no symptoms of varicose veins other than the visible appearance of the veins themselves.
However, while most varicose veins are harmless, some may indicate underlying health problems or have the potential to lead to complications.
It’s important to monitor varicose veins for any changes or concerning symptoms. Consult your GP or a vascular specialist if you experience:
- persistent pain
- swelling
- skin changes
- bleeding.
When should I seek medical attention for varicose veins?
While varicose veins are generally harmless, certain symptoms may indicate a more serious problem that requires treatment. Consult a healthcare professional if you experience:
- severe pain, aching, or swelling in the veins or lower leg muscles
- bleeding from the varicose veins
- skin changes, such as leg ulcers or sores that do not heal
- inflammation or redness around the varicose veins, which may indicate a blood clot (thrombophlebitis)
- difficulty walking or moving due to discomfort in your legs
- muscle cramp in your legs (especially at night).
What happens if I don’t seek treatment?
Ignoring varicose veins or delaying treatment can lead to complications. These can include:
- blood clots (deep vein thrombosis) that can travel to the lungs and cause pulmonary embolism
- chronic venous insufficiency, which can cause leg swelling, skin changes, and venous ulcers
- superficial thrombophlebitis, a painful condition characterised by inflammation of the veins.
Signs and symptoms to watch out for
While many people with varicose veins may experience no symptoms, others may notice some or all of the following symptoms:
- pain or discomfort (especially after prolonged periods of standing or sitting)
- swelling in the legs or ankles
- aching, throbbing, or heaviness in the legs
- itching or burning sensation around the veins
- skin discoloration or changes (such as redness or darkening)
- ulcers or sores on the skin near the varicose veins.
While varicose veins are rarely serious, if you experience pain, discomfort, or any of the symptoms above, it’s best to see your GP as soon as possible.
Expert tips for preventing varicose veins
Adopting healthy lifestyle habits and minimising risk factors can help to prevent varicose veins. Here are our expert prevention tips:
- Regular exercise – promotes good circulation and strengthens the muscles that support vein function. Activities such as walking, cycling, swimming, and yoga can improve blood flow and reduce the risk of varicose veins
- Weight loss – excess weight can put added pressure on the veins in the legs, leading to the development of varicose veins. Maintain a healthy weight through a balanced diet and regular exercise to reduce strain on the veins
- Move more – take breaks to move around and avoid prolonged periods of standing or sitting. Sitting for a long time can hinder blood circulation and contribute to the formation of varicose veins. If your job requires long periods of standing or sitting, try to incorporate regular breaks and gentle leg exercises into your routine
- Elevate your legs – keeping your legs above heart level for short periods throughout the day can help alleviate pressure on the veins and promote blood flow back to the heart. Aim to elevate your legs for 15-20 minutes several times a day, especially after long periods of standing or sitting
- Wear compression socks – these apply gentle pressure to the legs, helping to improve circulation and reduce swelling. Wear compression stockings during prolonged standing or sitting such as long flights or car rides
- Healthy diet – eat a diet rich in fibre, fruits, vegetables, and whole grains to maintain bowel regularity and prevent constipation. Limit the intake of high-sodium foods, as excess salt can cause fluid retention and swelling
- Avoid wearing tight clothing – particularly around the waist, groin, and legs. This can restrict blood flow and exacerbate symptoms
- Stop smoking – smoking can damage blood vessels and impair circulation, increasing the risk of varicose veins and other vascular conditions. Quit smoking to improve your vascular health
- Stay hydrated – drink plenty of water throughout the day to stay hydrated and promote healthy blood circulation. Avoid excessive consumption of caffeine and alcohol, as these can contribute to dehydration and worsen varicose vein symptoms
By incorporating these tips into your daily routine, you can effectively reduce the risk of developing varicose veins and promote overall vascular health.
Next steps
Whether you have vascular health concerns or are simply unhappy with the appearance of your varicose veins, don’t worry – there are several ways to treat them.
From lifestyle changes to minimally invasive procedures and surgery, your healthcare provider can recommend the most suitable treatment options. These will be based on your:
- symptoms
- medical history
- preferences.
If your GP thinks you could benefit from treatment, they may refer you to a vascular specialist or send you for a scan.
At Practice Plus Group, we offer affordable, private varicose vein treatment to help you feel more comfortable and confident. Talk to our team today to learn more.

Acknowledgements
Varicose veins FAQs
Not yet found the answers you’re looking for? Our dedicated varicose veins FAQs could help!
Yes, it is generally fine to live with varicose veins, as they are often a benign condition that do not cause significant health problems. Varicose veins are common, particularly among older people. While they may be unsightly or cause discomfort, they typically do not pose serious health risks.
Walking can be beneficial if you have varicose veins. It helps promote blood circulation and reduce symptoms. Talk to your healthcare professional if you’re not sure or need more information.
When you have varicose veins, there are certain activities and habits you should avoid. This is to prevent worsening of symptoms and reduce the risk of complications. You should avoid:
– prolonged standing or sitting
– wearing high heels
– wearing tight clothing
– smoking before surgery
– excessive sun exposure
– high-impact exercise
– delaying treatment if you have significant discomfort.
Varicose veins increase the risk of developing Deep Vein Thrombosis (DVT). This is a condition where blood clots form in the deep veins of the legs. If a blood clot breaks loose and travels to the lungs, it can cause a pulmonary embolism. This is a life-threatening condition.
If you’re worried about a blood clot, always seek medical advice.
Here are some signs to look out for:
– a blood clot in a varicose vein can cause localised pain or discomfort. This may feel like a throbbing or cramping sensation. The pain may worsen when standing or walking and may improve when resting or elevating the affected leg
– blood clots in varicose veins can lead to swelling around the affected area
– the skin overlying the varicose vein may appear red and feel warm to the touch. This is due to inflammation caused by the presence of the blood clot
– the area around the varicose vein may be tender or painful when touched. Gentle pressure may exacerbate the discomfort
– in some cases, a blood clot in a varicose vein may be visible as a firm, tender lump or cord-like structure beneath the skin. However, not all blood clots are visible externally
– if you have existing varicose veins and notice a sudden worsening of symptoms, such as increased pain, swelling, or redness, it may indicate the presence of a blood clot
It’s important to seek medical advice if you experience any of these symptoms. Blood clots in varicose veins can potentially lead to dangerous complications such as superficial thrombophlebitis or deep vein thrombosis (DVT).





